Disc pain in the back is commonly and perhaps erroneously referred to as a ‘slipped disc’ but what actually causes the pain and how can it be treated?
What happens to cause disc pain in the back?
This is the most painful and debilitating thing to go wrong in the back. The disc is a fibrous plate that sits between the round bony bodies of the vertebrae. They are fibrous around the outside and jelly like in the middle - like a doughnut. These cause bigger acute issues when you are younger with bulges and splits. However, the jelly turns to fibre as you go through your 40’s so these are less likely as you get older.
The main problem is that the disc splits, bulges or leaks. This is painful and a decent size bulge can press on the nerves just behind the disc and cause more pain and referred nerve symptoms like pain, pins and needles, weakness and numbness in the leg.
Symptoms of disc pain
Typical symptoms are a debilitating pain in the lower back and a lot of spasm in the muscles, tightness and pain in the bum and nerve symptoms in the back of the leg.
If you have spine or back pain and experience any change in your bowel or bladder control you should contact your GP or Accident and Emergency immediately for further investigations and/or advice.
How to test your symptoms
The presence of leg pain to the knee or below is usually an indication of a disc issue.
Discs pain is typically:
- Worse to sit and bend forwards than to stand or lay
- Painful standing up from sitting
- Painful in certain positions at night
- Particularly bad in the morning for a couple of hours
- Terrible when coughing and sneezing
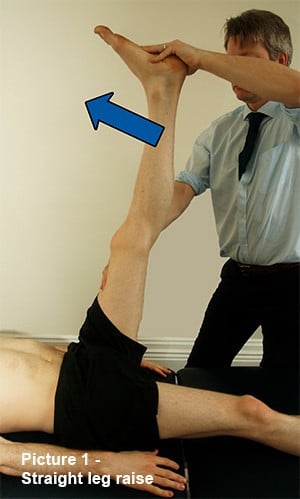
If there is pain on straight leg raise it is a sign that the nerve is being pressed. This means that when your affected leg is taken up as in Picture 1. The range available on the affected leg is at least 20 per cent reduced by pain when compared to the other side.
This test is painful in a disc issue so take care when using it by lifting slowly from flat and stopping at the onset of pain.
How to treat it
This depends on how it started. If it was an acute onset – so a lift and an ‘ouch’- then the initial treatment is to rest for a couple of days or so to allow the acute inflammation to settle down. This is not complete rest but lay down at least 20 minutes per hour and then get up for a short walk or a few exercises.
The simplest and most effective two exercises when the back is in the acute phase are:
- ‘Extension’
- ‘Rotation’
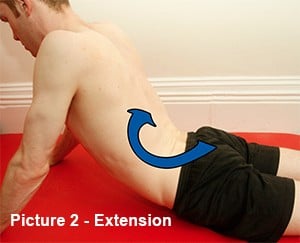
For extension (see Picture 2,) you need to lay face down and use your arms like you are doing a press up. However, your tummy stays in contact with the floor and you arch the back. Do not use your back muscles, but try to relax them. Only move as far as is possible in comfort. Repeat 15 times for a couple of sets every hour.
The rotational stretch (Picture 3) is performed with the most painful side of the back uppermost. Keep the shoulders relatively flat and turn your hip well underneath you. Bring the top leg over and help with your hand. Have the lower leg straight. Turn as far as is comfortable and rock for 20 seconds and repeat 6 to 10 times increasing the distance each time if possible.

The mistake made here is to not take your hip far enough underneath you. Whilst the shoulders are flat you need to turn the hip far enough to be laying on your hip bone. (Greater Trochanter)
Timescales for recovery
An acute disc prolapse will take from a few days to 6 weeks to resolve. After the first few days you will be feeling a bit more mobile and less sore. If you are making tangible progress then keep going.
However, if you are not feeling better then seek help from your GP for drugs to help relax the muscles, reduce the inflammation and control the pain. These can be more effective than over the counter drugs for the level of pain associated with a disc issue. It is also not the time to be a martyr. Taking the drugs helps the body to heal and you more comfortable.
As you become more mobile you can start to be more active. The disc is starting to heal. However it is still fragile – think of it as a newly formed scab. Avoid movements that hurt. This is when the ‘scab’ is being stressed and potentially damaged causing more pain and a delayed healing process.
Exercise like easy swimming and walking are most useful, within pain levels. Avoid sharp pain whilst an ache is acceptable.
The key thing here is to remain positive and understand that whilst it is painful they do resolve, you will resume an active life, and you won’t necessarily have a problem for ever.
Physio Treatment
Physio treatment has been proven by quality clinical research to be very effective in the treatment of low back pain.
If the back pain does not start to settle in 4-6 days then seek help from your physiotherapists as well as the GP. There is much that can be done and also ensuring you have the right diagnosis and thus treatment is hugely helpful.
Physiotherapy should constitute a full assessment and manual work to restore ranges and reduce spasm. There will be advice for the self-treatment and a decision as to whether there needs to be referral for investigations such as MRI.
Guidelines for the treatment of lower back pain from NICE (National Institute of Clinical Excellence) show that there is little benefit in an early MRI as it does not alter the treatment of choice which is rest, exercise and physiotherapy. However, your physio will help you through this process and communicate with your GP as required.
For more information on lower back pain injuries, visit our 'Introduction to lower back pain' article.














