Plantar fascia is a common issue in runners, especially with track work and hilly runs. Find out the causes, symptoms and treatment for plantar fasciitis from physio Mark Buckingham.
What is the plantar fascia?
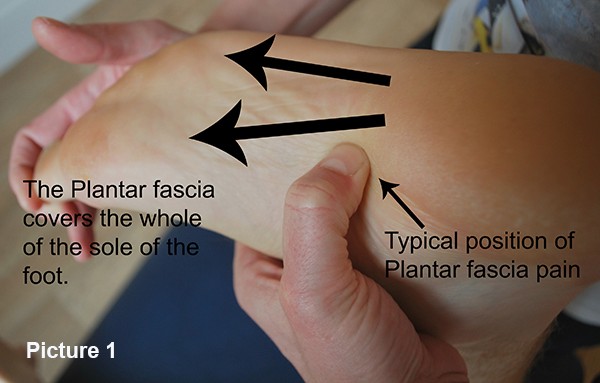
The plantar fascia is a fibrous band which spreads across the sole of the foot from the toe to the heel. It attaches from all the toes and across the base of the heel. The typical site of pain is on the inside edge of the heel (as shown in Picture 1.)
Plantar fascia is generally caused by the foot rolling in and applying too much pressure and force to this area. This type of overload causes strain, micro-tearing and laying down of scar tissue. This gradually becomes more inflexible and eventually becomes chronically inflamed and thickened.
The cause of the poor biomechanics can be from a number of sources but commonly tight calves and weak foot invertors (tibialis posterior) as well as poor glute control and strength.
The pain can be intermittent and excruciating and has been described from a burning sensation to a feeling of a nail being driven into the heel!
The discomfort is usually worse in the morning when getting out of bed or after long periods of inactivity. This is because the scar tissue stiffness up is given the opportunity and takes longer than normal tissue to become flexible. It is this stiffness that makes the area sore to begin running. As it warms up it might become less painful but typically then becomes tired and sore. After running it will then tighten up considerably and can be sore to walk.
Diagnosis is based around location and pattern of behaviour. A more constant ache at rest/ night has concerns for bone stress issues so be aware of these.
Treatment for plantar fascia issues
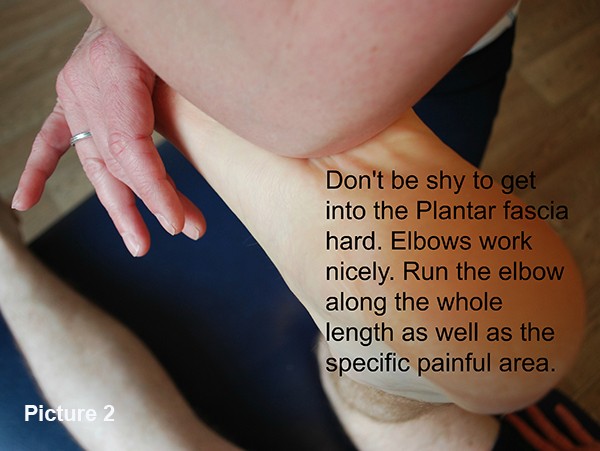
There are several lines of focus here. The tissues have to be altered to make the scar tissue much more flexible and to improve the strength. To work into the arch in the foot is very useful – either with an elbow (as shown in Picture 2), or a golf ball. A couple of minutes are needed and twice a day is enough. This needs to be firm enough to change the structure of this scarring and thus is it quite sore. It will warm up during the process and as the scar tissue improves over a few weeks then it will become almost pain free. This is a good indicator that you have made good progress.
Beyond the local scarring you need to look at why you are overloading the tissues in the medial arch of the foot. The most important area is weakness of the foot invertors – Tibialis Posterior. This hugely important muscle holds the arch up and decelerates the rolling in of the arch of the foot on impact (pronation).
However, a full biomechanical assessment is essential and the tests for this is are detailed in the Biomechanics Sections .
Simple self-tests can be useful. Stand in front of a mirror and perform a single leg knee bend. Watch where your knee aligns over your foot. The knee should stay over the middle of the foot and the foot should not roll in. Look at a hop in the same way.

If it is poor look at four things:
1. TP strength
Hold the foot as shown. You should be able to hold your foot against a person trying to push your foot outwards (as in Picture 5.) Compare to the non-symptomatic side.
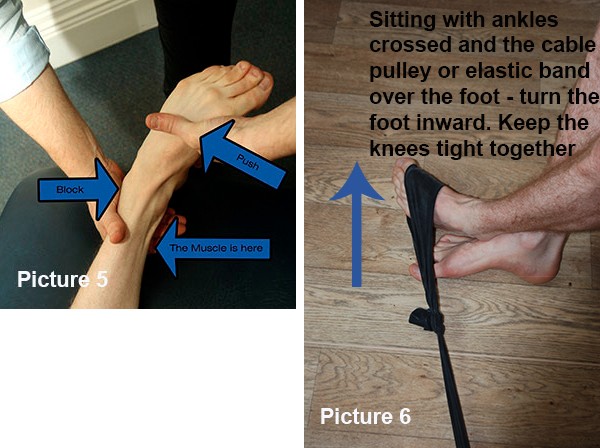
If you cannot hold the foot solidly then you need to strengthen. Simple work with a TheraBand will help. See Picture 6. 3 times 15 reps at a resistance where 15 is very tired. You can do this same exercise with a cable pulley. Use a 8 reps, 4 sets protocol.
2. Calf length
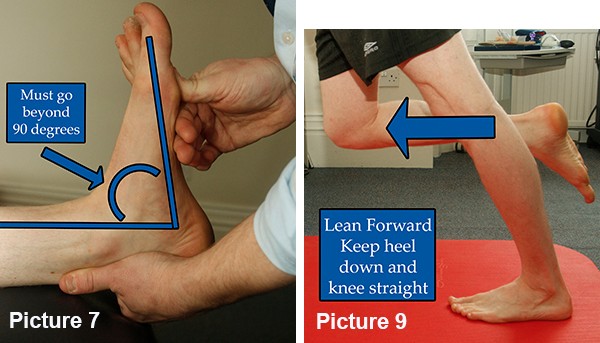
Tightness may or may not be an issue but normal length gives at least 20 degrees of easy dorsiflexion range past 90, as shown. The foot should not want to move to the outside as you push it up (as in Picture 7.)
Rolling the calf is the most effective way to lengthen the tissues (Picture 8.) Normal calf stretching (Picture 9) is also effective but the lower fibrous part of the calf is less receptive. Stretch and roll for 2 minutes, 4 times a day. When stretching the calf ensure the foot is in line with the knee and the arch held high.

_
3. Lateral Gluteal strength
The lateral gluts are responsible for holding the knee over the foot. In the test position shown in Picture 10, hold the leg up behind the line of the body. The tester should not be able to push the leg down. Compare to the other side. If the leg can be pushed down then the lateral glutes are too weak.
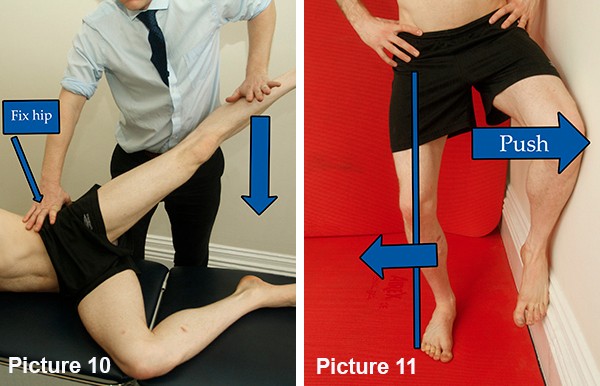
A simple way to begin to strengthen the lateral glute is by standing with the affected leg outermost from a wall and the other knee up against the wall (as in Picture 11.) Bend the standing knee to just in line with the toes and turn it out over outside of the foot. Push the wall leg into the wall and brace using the glutes on the standing leg. Try to hold it for a minimum 2 minutes and build to 5 minutes.
Calf strength
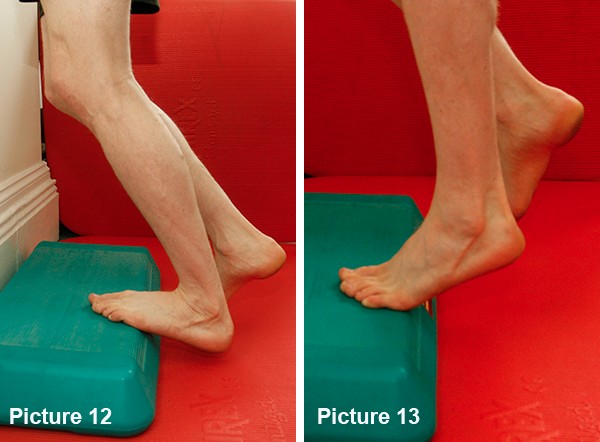
Whilst not directly related to alignment, calf muscle strengthening is essential in Plantar Fascia issues. The PF is connected to the calf muscle in terms of tissues as well as function and a weak calf will absorb force poorly. Calf strength work off a step will also load the PF tissue and increase its tensile strength in the same way that these exercises will improve the quality of the Achilles tendon. It is the same sort of fibre after all.
Stand on a step and lower the heel completely off the edge, bending your knee into it, before rising fully up to tip toes. Repeat this for 25 reps, 3 sets. To start this will be tough so do as many as you can and build up (see Pictures 12 and 13.)
Time scale for recovery from plantar fascia issues
Recovery from plantar fascia issues can take some weeks due to the amount of change that must occur in the tissues and how poor those tissues are at this change due to poor blood flow. If you have worked at this protocol for more than three weeks and seen no change then please seek further help from a running specialist Chartered Physiotherapist.














